
Quality & Safety
The Role of Medical Radiation
There was a time when the only way a physician could look inside a patient was through the most direct route available—invasive surgery. Today, physicians turn to advanced medical imaging procedures, such as computed tomography (CT), PET/CT, interventional radiology, and image-based surgical procedures to aid in the early detection, diagnosis and treatment of cancer, cardiovascular, neurological disease, and other health conditions.
As a result of earlier and improved diagnosis, survival has increased, recovery times have decreased, and overall quality of patient care has improved.
Most of us can look to our own experiences as proof of the value of medical imaging:
- A screening mammogram that identified a mother’s early stage breast cancer
- A visit to the emergency room where a CT scan allowed the physician to make a diagnosis of acute appendicitis
- A grandfather’s CT angiography that helped identify major reductions in blood flow to his heart
- A friend’s interventional procedure to decrease the pain associated with her abscess
- A father, aunt, cousin or colleague whose virtual colonoscopy scan identified a pre-cancerous polyp.
The examples above describe the importance of imaging procedures that use radiation. But some imaging procedures such as ultrasound and magnetic resonance imaging (MRI) do not involve radiation.
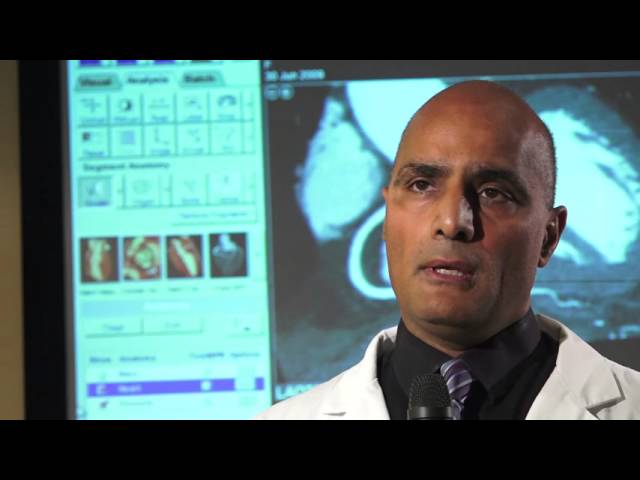
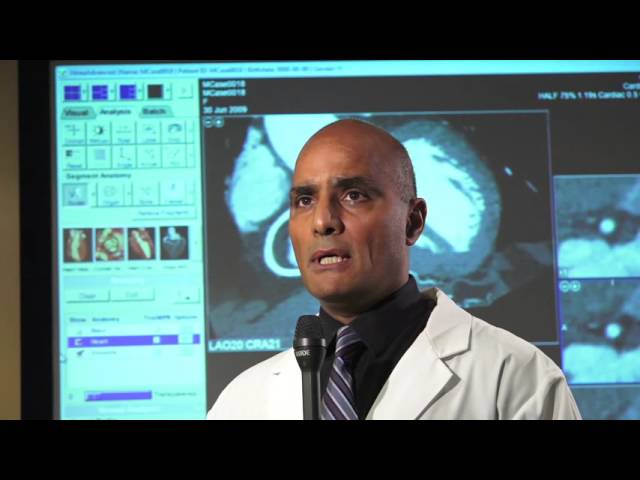
“The whole issue of radiation dose safety is something that radiologists take very seriously. We want to make sure we are using the lowest radiation dose possible.”
So why is radiation necessary for some procedures and not others?
The answer lies in the technology. Various imaging methodologies, such as CT scans, MRI, nuclear medicine scans, and ultrasound, generate images in different ways. X-rays were one of the first ways to see inside the human body, and the technology remains valuable today.
Determining which imaging method is the best one to use in any particular circumstance is based on a number of factors, including the clinical status of the patient, the goal of the imaging study, the level of detail needed and whether anatomical information is sufficient or if functionality is also necessary. These are just a few of the considerations that enter into the decision-making process when a physician or other healthcare provider orders an imaging procedure.
Medical professionals and their patients should discuss treatment goals and options to decide on the appropriate imaging technique.
Ontario radiologists are committed to the philosophy of the right image using the right amount of radiation, for the benefit of the patient.
The OAR wants you to know more about the benefits and potential risks of radiation used in medical imaging. By supporting informed decisions that are based on both the benefits and the risks, we are working to help ensure that medical imaging continues to be an appropriate, powerful tool in the detection, diagnosis, and treatment of illness and disease.
Radiation in Medical Imaging Has Its Benefits
For a brief snapshot that shows the power of medical imaging, consider these findings:
- Use of mammography to screen for breast cancer has resulted in a declining death rate, improved survival rate, and better treatment options
- Performing coronary CT angiography to examine the heart vessels in patients with chest pain helps guide treatment decisions with high accuracy and avoids costly invasive procedures
- Incorporating advanced medical imaging procedures into healthcare has significantly increased life expectancy in Canada
ALARA (As Low As Reasonably Achievable)
Ontario Radiologists subscribe to the ALARA principle with recommendations to minimize one’s exposure to radiation to the lowest level possible, such as choosing alternate imaging methods (if appropriate), increasing the distance from the source of radiation, decreasing exposure time and using the right shielding, if appropriate.
“In Ontario in particular, we have been very strong in the field of radiation dose reduction. In 2006, we published the first worldwide study showing that patients at Princess Margaret Hospital with leukemia could be examined with low dose CT.”
Radiation in Medical Imaging Has Its Risks
Almost all medical procedures, including imaging procedures that use radiation, have risks associated with them. Physicians and patients should carefully consider the potential benefits and the risks when considering the use of imaging techniques that involve radiation.
Each patient’s clinical situation is different, but here are some things for healthcare providers to consider when deciding whether or not an imaging procedure that uses medical radiation is the right choice.
In determining the appropriate test for patients, physicians consider a number of issues:
- What is the purpose of the procedure? Is it to arrive at a diagnosis, assess treatment response, or is it preventive screening?
- Are there alternative imaging procedures that could accomplish the same goal without medical radiation, such as ultrasound or magnetic resonance imaging?
- What are the risks of not having the imaging procedure done?
- How old is the patient? The risks for pediatric and adolescent patients may be different than for adults.
- Is the patient pregnant, possibly pregnant, or breastfeeding?
- What other procedures is the patient likely to undergo during this workup?
- What is this person’s radiation exposure from previous medical procedures? For example, has the person undergone multiple CT or nuclear medicine scans in the past?
- What is this person’s occupational exposure to radiation, if any?
- Will the imaging exam be performed on low-dose equipment?
Healthcare providers and their patients are encouraged to discuss these issues and any other potential risks with the treatment team, including the radiologist in charge of supervising the imaging procedure.





