CBMD Facility Accreditation Frequently Asked Questions & Answers
Question:
What is the cost of the CBMD Facility Accreditation Application?
Answer:
The cost of CBMD Facility Accreditation Application is $2,000 (two thousand dollars) per DXA unit.
Question:
What does the $2,000 Application Fee cover?
Answer:
The $2,000 Application Fee covers the following:
- Cost of the medical physicist’s visit
- Review of the application by the CBMD Review Team
- Processing of application and CBMD Facility Accreditation Certificate
- The CBMD accreditation is now for five (5) years, where previously it was for three (3) years.
Question:
Are anniversary reviews still required during the accreditation and are the costs of the physicist’s reviews covered in the $2,000 application fee?
Answer:
Yes, anniversary reviews are required beginning with the first anniversary year. The cost of the anniversary review is the responsibility of the hospital/facility and paid to the CBMD approved physicist. The cost of each anniversary review is $400.
Question:
What is required for the anniversary review and how will sites be notified that a review is pending?
Answer:
Note: Once a site has been accredited, a physicist’s visit to your facility is not necessary until the accreditation renewal in five years time. The exception is if there has been a major change such as a machine or tube replacement, etc., in which case, a physicist visit is required.
The site must send the following materials to the OAR’s CBMD medical physicist at the first, second, third and fourth anniversary of your accreditation approval so that your CBMD physicist may review:
- The maintenance records of the BMD machine(s). Any major changes, maintenance and repairs should be highlighted such as tube replacement or major software upgrades, any re-location of the DXA scanner, and BMD equipment replacement. As noted above, this information should be immediately communicated since it may require a physicist visit.
- Copies of the year’s Shewhart BMD and area plots and a summary of action taken if any of the Shewhart rules were violated.
- All information on any changes in technologist staff and their precision data. This should include both the addition and the deletion of staff doing BMD testing.
The OAR CBMD online system will automatically send sites notice of their anniversary requirements and due dates.
Sites will be invoiced by their medical physicist for the anniversary review.
Question:
How does a hospital or clinic get a CBMD physicist?
Answer:
The OAR will assign a CBMD Program medical physicist once the facility accreditation application fee has been processed. Sites must use the CBMD approved medical physicist assigned by the OAR. Medical physicists within the CBMD program have been specially trained and are the only physicists whose work will be accepted for the program.
Question:
How/when will our facility gain access to the CBMD Facility Accreditation Online Application?
Answer:
Once the application fee has been processed, the facility will receive an email notification of acceptance along with instructions on how to access the online application.
Question:
Is there a discounted fee for accrediting multiple DXA units?
Answer:
No. The application fee for each unit is $2,000 and a separate application is needed for each DXA unit.
Question:
Are all technologists working in BMD required to do the precision testing?
Answer:
Yes, all technologists are required to do their precision testing. Results are averaged for the department / clinic.
Question:
What qualifications are required by the CBMD Facility Accreditation Program for physicians and technologists providing BMD services?
Answer:
Reporting Physician
The examination must be performed under the supervision of and be interpreted by a licensed physician with the following qualifications:
- Is certified by the Royal College of Physicians and Surgeons of Canada or by the Collège des Médecins du Québec as a specialist.
- Is a member in good standing with the College of Physicians and Surgeons of Ontario (CPSO).
- Is licensed to practice medicine with the Province of Ontario with an Ontario billing number.
- Has documented training in bone mineral densitometry and osteoporosis. Documented training can include:
- Specialized residency training or a mini-fellowship in BMD
- Various BMD courses plus literature “reads”
- At a minimum, participation in one of the CBMD Facility Accreditation Seminars or Workshops and a commitment to taking ongoing CME training.
- Continuing professional development for the physician(s) concerned shall be according to current Canadian Association of Radiologists’ (CAR) and Royal College of Physicians and Surgeons of Canada Maintenance of Competence Guidelines.
- Maintains 15 hours of Continuing Medical Education (CME) in clinical densitometry as set out in the CBMD CME guidelines (7.5 hours of which may be self-education) over 5 years.
- Possesses detailed medical imaging knowledge and understanding of bone, structure, metabolism, and osteoporosis.
- Documented training and understanding of the physics of X-ray absorption and radiation protection, including the potential hazard of radiation exposure to both patients and personnel.
- Knowledge and understanding of the process of DXA data and image acquisition, including proper patient positioning, placement of regions of interest, and artifacts or anatomic abnormalities that may falsely increase or decrease bone mineral density value.
- Knowledge and understanding of reporting parameters, including, but not limited to: bone density measurements, percentage of mean, T-Score, Z-Score, fracture risk, and the World Health Organization (WHO) classification system.
- Detailed knowledge and understanding with respect to the reporting of BMD using the “Canadian Association of Radiologists Technical Standards for Bone Mineral Densitometry Reporting”, Siminoski et al, CARJ 64 (2013) 281-294.
- Knowledge and understanding of the criteria for accurate and precise comparison of serial measurements, including limitations of comparing measurements made by different techniques and different devices.
- Knowledge and understanding of other techniques for bone density measurement to ensure that the physician is able to fulfill a consultative role.
- If plain radiographic images are obtained to correlate with BMD studies, physician qualification should be in accordance with the CAR Standard for General (Plain) Film Radiography.
- The physician must be familiar with the methods and statistical analyses necessary for the determination of site and machine specific precision.
- The supervising physician shall be responsible for oversight of the DXA facility, technical staff, and equipment quality control program. The reporting physician accepts final responsibility for the quality of all BMD exams used in reporting.
Technologist
- The technologist shall be certified in medical radiation technology by the Canadian Association of Medical Radiation Technologists (CAMRT).
- Be a member in good standing with the College of Medical Radiation Technologists of Ontario (CMRTO), or other provincial licensing body as appropriate.
- Comply with the requirements of continuing education as set out by the CMRTO and CAMRT. In addition, the technologist shall be an Accredited Densitometry Technologist (ADT), or equivalent training recognized by the CBMD.
- The technologists will be responsible for:
- Patient comfort and safety
- Patient preparation
- Proper patient positioning
- Monitoring the patient during the measurements
- Obtaining the measurements prescribed by the supervising physician
- Placement of the region of interest (ROI) of bone mineral density measurements
- The technologist will have documented training in the use of the DXA equipment, including performance of all manufacturer-specified Quality Assurance (QA) procedures. In addition, training should meet the level of excellence set by the OAR’s CBMD Facility Accreditation program.
- The technologist must read, be familiar with, and have access to the manufacturer’s operator manual for the specific scanner model being used.
- The technologist is encouraged to participate in patient education of osteoporosis.
- If plain radiographic images are performed to correlate with DXA studies, the technologist's qualifications must be appropriate.
- The technologist must meet requirements for Continuing Education (CE) as established by the CBMD Facility Accreditation Program, which is a minimum of 35 hours CE, (7.5 hours of which may be self-education) over five years at the time of re-accreditation.
Note: Copies of licenses for all technologists, and certificates and other documentation of continuing education for all technologists involved in bone densitometry examinations must be routinely updated.
Question:
Is it necessary to scan the Spine Phantom on every clinical day?
Answer:
Yes. The phantom must be scanned at the beginning of every clinical day and the results must be analysed for any violations of the Shewhart rules.
Question:
Why does the bone densitometer need to be inspected every year? If QC is performed and within spec daily, if no software changes have been made and if regular maintenance is performed to monitor equipment performance. What is the advantage of yearly inspection?
Answer:
The physicist visit is only once every five years, however, annual reports on QC data are necessary to show that equipment is being maintained. This requirement is similar to that of the Ontario Breast Screening Program. The physicist will review this data and issue a report. He/she will keep a copy on file for future comparisons, send one to the facility and upload one to your CBMD Online application file. Sites should consult with their physicist regarding questions about equipment and QC data.
Question:
At the CBMD course, technologists were instructed to compare femoral total BMD for interval change and not the femoral neck BMD. How do me make use of the femoral neck LSC?
Answer:
For clinical practice, LSC only needs to be determined for total hip and total spine (L1 to L4), since these are the two regions used in reporting changes in density. The hip sub-regions, including the femoral neck, are not used in clinical practice in monitoring changes in density. Rather, the sub-region precision determinations serve a quality control purpose to verify that there is not excessive error in any component that contributes to the total hip value.
Question:
Is there a recommended or required number of scans a BMD technologist must/should perform to remain competent? Details are clear for obtaining accreditation, but are there ongoing requirements to maintain competency?
Answer:
A minimum number has not been established. The CBMD program is more concerned with a technologist maintaining quality control and quality assurance procedures and monitoring their precision.
A technologist who must scan a large number of patients with little time to assess each individual exam to ensure that positioning, technique, ROI, areas etc. have all been maintained, will not perform as well as a tech who scans fewer patients, but has the time to properly monitor the patient exams.
It is true that scanning technique improves with time as does the scanning of more patients.
The key is to determine a technologist’s precision through a precision study on a representative patient population and then to monitor this precision to be sure it is maintained.
Question:
How should technologists scan a patient who has had bilateral hip replacements? We have heard that technologists must scan two sites: lumbar spine and wrist, or hip and wrist…is this correct?
Answer:
You should only scan the spine, plus do an X-ray of the lumbar spine to assess for vertebral fractures.
Scanning the distal radius has some value in diagnosis in clinical situations such as hyperparathyroidism, but is not really helpful in fracture risk assessment!
Question:
When doing a precision study, can a patient be irradiated for the same procedure 2 to 3 times without an order for additional tests? Would a standing order cover the situation?
Answer:
The repeat scans are necessary for precision studies. These values are used to calculate the LSC for your site. A consent form may be obtained to perform the extra scans necessary to achieve the precision study. The patient should be informed about the very low dose of radiation involved and the benefits of the precision study in monitoring patients.
Question:
What is the term of my accreditation and do I need to submit any additional information once I have been approved?
Answer:
The CBMD Facility Accreditation is for a five-year term. As part of your accreditation your site will be required to submit the follow-up reports at the annual anniversary of the accreditation approval. These reports are to be submitted to the Ontario Association of Radiologists.
Maintenance records of the BMD machine(s). Any major changes, maintenance and repairs should be highlighted such as a tube replacement or major software upgrades, machine moves and BMD equipment replacement.
Copies of the year’s Shewhart and area plots and a summary of actions taken if any of the Shewhart rules were violated.
All information on any changes in technologist staff and their precision data. This should include both the addition and the deletion of staff during BMD testing.
Question:
Is it necessary that I scan the Spine phantom every clinical day?
Answer:
Yes. The phantom must be scanned at the beginning of every clinical day and the results must be analysed for any violations of the Shewhart rules.
Question:
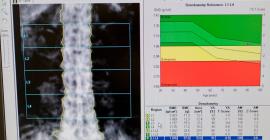
What are Shewhart rules?
Answer:
These are rules that govern the type and number of deviations that are allowed for the phantom BMD result before the patient testing must be stopped and the DXA unit serviced and corrected. These rules can be found in the physics report or in Sidney Lou Bonnick, Bone Densitometry for Technologists. Humana Press. New Jersey, 2002.
Question:
Is the graph and data on the DXA machine for phantom tests sufficient?
Answer:
No. These results are not adequate and do not follow the Shewhart Rules. Thus the daily phantom data needs to be analysed using the Shewhart Rules.
Question:
How do I get my baseline for the Shewhart plot?
Answer:
The baseline is established for at least 30 spine phantom scans (L1-L4) over the last year of operations. Note: do not use multiple scans from the same day but use scans spread out as much as possible over the last year.
Question:
What do I do if Shewhart rules are violated?
Answer:
If the rules are violated, make sure that the test is accurate by trying it again and if it still fails stop the patient procedures and have the machine repaired and re-calibrated.
Question:
Can the baseline change over time?
Answer:
The baseline should not be changed under normal operating conditions. Only under special circumstance of major change such as, major repairs/upgrades or change of equipment can the baseline change. Under these conditions crossover precision testing needs to be done.
Question:
What do I do before starting major repairs on the equipment in order to maintain precision?
Answer:
If repairs or upgrades are planned, do 10 phantom scans before the work is started and then 10 scans after the work is completed. Compare the results before and after the repairs and if they do not match the system must be calibrated. Note the phantom must be removed and re-positioned for each scan. If the machine breaks down unexpectedly then do the 10 scans after the work has been completed and compare to the existing baseline. If the results do not match the system must be re-calibrated. After re-calibration the phantom tests on following clinical days must hover around the baseline in a similar manner as the data from tests before the service/upgrades. If this fails and re-calibration is unsuccessful, precision crossover testing needs to be done.
Question:
What is crossover precision testing?
Answer:
This is the establishment of a crossover of the least significant change (LSC) value. Choose 30 patients from the last 30 days before the repairs/upgrades and scan them again each 2 times as would be done in standard precision testing. Then take the patient’s previous scan and the first of post repairs/upgrades scans and enter these into the precision calculator. Now you have calculated the crossover LSC. Take the two-post repair scans and enter them into the calculator and this provides the regular LSC. The crossover LSC must be used for all patients that have had their previous scan on the pre-repaired system and the subsequent scan under the repaired system. For any patient with both scans on the repaired system use the regular new LSC.
Question:
How do we combine the precision results for facilities with multiple technologists?
Answer:
This is still an area of further study but for now the results for multiple technologists should be averaged.
Question:
Should the LSC be reported as an absolute value or percentage?
Answer:
The LSC must be reported in g/cm2. It must be a unique determination of LSC reflecting the precision of the equipment and technologist staff.
Question:
When trying to determine the BMD in the spine, (where values from L1 to L4 have a fair bit of ‘artefact’ eg sclerosis, tilt), should L1 to L4 be reported using the T-score from the best two for the diagnostic category?
Answer:
When determining the diagnostic category or fracture risk with respect to the spine, a single vertebra cannot be used. A minimum of two contiguous valid vertebrae between L1-L4 is required. These guidelines are outlined in the June 2005 article “Recommendations for Bone Mineral Density Reporting in Canada”.
Question:
Is there proper authorization for technologists to be irradiating a patient two or three times for the purposes of establishing precision in BMD testing? Does this contravene the ALARA principle?
Answer:
The radiation dose to patients participating in precision testing is very small and within the scale of the natural variations in background radiation exposure depending on the geographical location and altitude. The dose from natural background radiation in most places at sea level is approximately 2,500 µ SV/annum (or about 7 µ SV/day). Using the ICRP methodology the effective dose for a routine DXA scan of the hip and spine would be typically less than 10 µ SV.
Precision testing is not considered research and therefore does not require the approval of the institutional ethics committees. Patient involvement should be via informed consent. Each participating patient benefits from precision assessment as it contributes to improve the interpretation of results. It is also reasonable to argue that it would be unethical to not perform precision testing as the lack of precision testing would result in a misinterpretation of results and be a cause of potential therapeutical issues.
Question:
Can a patient be irradiated for the same procedure two to three times without an order for the additional tests? Would a standing order cover the situation?
Answer:
Permission from the patient must be obtained to perform the extra scans necessary to achieve a precision study. The patient should be informed about the very low dose of radiation involved and advised that the precision study will be a benefit to the patient as well as other patients so that the follow-up DXA scans at the facility will have some meaning and value in monitoring patients.
Subsequent Question:
If a technologist goes through all the time and effort of determining precision at the time of initial accreditation but then only scans one evening shift per (week or possibly even less) will the technologist lose competency? Is there no requirement for repeat assessment of precision until accreditation renewal is due?
Answer:
It is correct that having too many technologists involved in scanning will affect the quality of the program. The CBMD Advisory Committee has made this clear. Increasing the number of technologists involved will affect site precision and also decrease the individual techs learning curve with respect to improving scanning technique.
The ideal situation, which is often impossible to achieve is having the patient scanned on all occasions on the same machine by the same technologist. Recognizing that this is impossible to achieve in larger centers an attempt should be made in the interest of patient care to work with the minimal number of technologists. It becomes extremely difficult to maintain quality assurance in terms of feedback to technologists when there are increasing numbers of technologists scanning. It should also be realized that if you have ten technologists each must do their own precision study.
The CBMD Advisory Committee has not identified any specific ratio of technologists per DXA unit except to reinforce the above principles. At the time of an accreditation process the physicist should be helpful in reviewing facility policies in this respect and making appropriate recommendations where matters affecting quality assurance are identified.