The OAR is continuing to advocate for patients and radiologists and is committed to working with the Provincial Government to find solutions.
Mammography is a specific type of imaging that uses a low-dose x-ray with high-contrast, high-resolution film for examination of the breasts to assist in the detection of breast diseases. The images of the breasts can be viewed on film at a view box, or as soft copy on a digital mammography workstation. Most medical experts agree that successful treatment of breast cancer often is linked to early diagnosis. Mammography plays a central part in early detection of breast cancers because it can show changes in the breast up to two years before a patient or physician can feel them.
“Breast screening absolutely makes a difference; with screening mammography we are routinely able to diagnosis cancers. With screening mammography we are routinely able to diagnose cancers that are small, they are treatable and the treatment options increase.”

The OAR supports the initiatives of Cancer Care Ontario and the Ontario Breast Screening program (OBSP) and is working with radiologists and technologists to find new ways to detect breast cancer in its earliest stages. Breast cancer screening is the regular examination of a woman’s breasts to find breast cancer early.
- A mammography unit is a rectangular box that houses the tube in which x-rays are produced.
- The unit is dedicated equipment because it is used exclusively for x-ray exams of the breast with special accessories that allow only the breast to be exposed to the x-rays.
- Attached to the unit is a device that holds and compresses the breast and positions it so images can be obtained at different angles.

- The breast is exposed to a small does of radiation to produce an image of internal breast tissue.
- The image of the breast is produced as a result of some of the x-rays being absorbed, while others pass through the breast to expose either digital image receptor (full-field digital mammography) or film (conventional mammography, which is limited to 40 sites in Ontario).
- The images are digitally stored on computer, or exposed film is placed in a developing machine – producing images much like the negatives from a 35 mm camera.
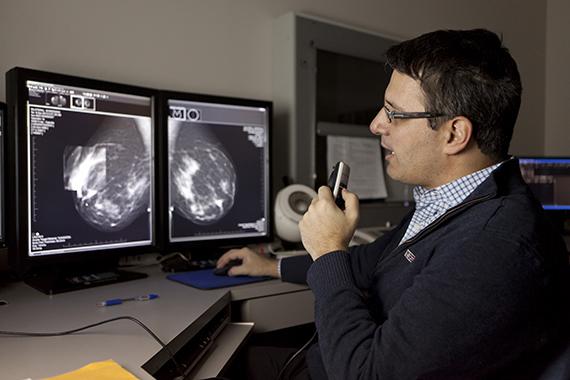
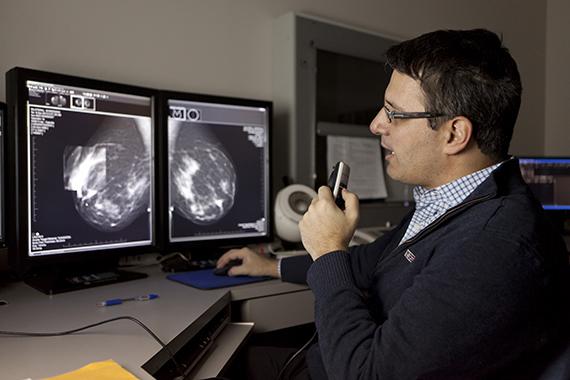
- A radiologist, who is a physician experienced in mammography and other x-ray examinations, will analyze the images, describe any abnormalities, and suggest a likely diagnosis. The report is dictated by the radiologist and sent to the referring physician.
- It is important to note that the OAR continues to advocate for full access to digital mammography for all Ontario women and has been championing this cause for many years in Ontario.
- This critical access to state-of-the-art care issue is also being incorporated into the OAR’s new public education campaign.

During mammography, a specially qualified radiological technologist will position you to image your breast. The breast is first placed on a special platform and compressed with a paddle (often made of clear Plexiglas or other plastic). Breast compression is necessary in order to:
- Even out the breast thickness so that all of the tissue can be visualized;
- pread out the tissue so that small abnormalities won’t be obscured by overlying breast tissue;
- Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged;
- Hold the breast still in order to eliminate blurring of the image caused by motion;
- Reduce x-ray scatter to increase sharpness of picture.
The technologist will go behind a glass shield while making the x-ray exposure, which will send a beam of x-rays through the breast to the film behind the plate, thus exposing the film. You will be asked to change positions slightly between images. The routine views are a top-to-bottom view and a side view. The process is repeated for the other breast. The examination process should take about half an hour. When the mammography is completed you will be asked to wait until the technologist examines the images to determine if more are needed.
- You will feel pressure on the breast as it is squeezed by the compressor.
- Some women with sensitive breasts may experience discomfort. If this is the case, schedule the procedure when your breasts are least tender.
- The technologist will apply compression in gradations. Be sure to inform the technologist if pain occurs as compression is increased. If discomfort is significant, less compression will be used.
- After your screening mammogram is completed a radiologist specializing in mammography will interpret your films.
- The radiologist will study, or “read” your films and identify any abnormalities or “findings”.
- The radiologist will also utilize the computer aided diagnosis (CAD) system which acts as a second pair of eyes.
- The radiologist will issue a radiology report to your referring physician and a letter with your results will be mailed to you.
- If additional tests are necessary, you will be notified by your physician to return for a diagnostic mammogram and/or a breast ultrasound exam.
- A diagnostic mammogram is read in real-time by the radiologist, and you will be given your results before you leave the facility.
- Mammography (breast x-ray) remains the best screening test for most women.
- A screening mammogram is usually for a patient with no history of breast problems or symptoms and is a central part in early detection of breast cancers.
- It is performed by highly skilled mammography technologists and interpreted by a certified radiologist specializing in mammography.
- A written report with the results of this exam will be sent to you and your physician. You are not examined or seen by a radiologist.
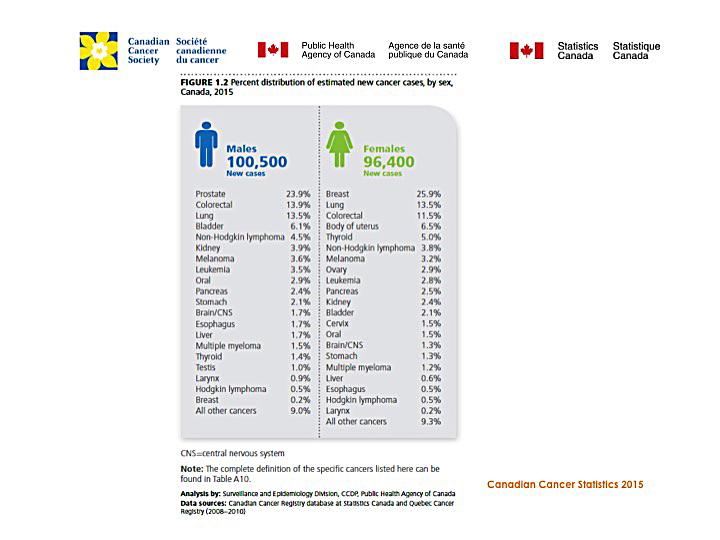
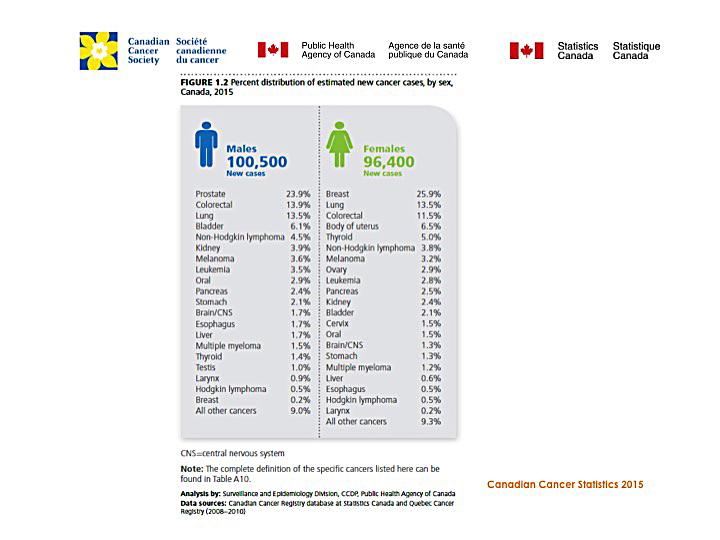
- In Ontario, breast cancer is the most common type of cancer in women.
- As they get older the chancer of getting breast cancer rises. Mammograms can help to find small breast cancers before there are symptoms. If breast cancer is found at an early stage there is a high rate of successful treatment. Finding cancer early may allow for more treatment options, such as breast conserving surgery or less aggressive treatment.
- Breast cancer screening saves lives. Between 1990 and 2008, breast cancer death rates in Ontario women aged 50–74 decreased by 37% due to improved cancer treatments increased participation in breast cancer screening, and a recent decline in breast cancer incidence.
- Regular breast cancer screening can find cancer when it is small, which means: there is a better chance of treating the cancer successfully. It is less likely to spread. There may be more treatment options. Ontario women can receive a screening mammogram in one of two ways: through Ontario’s organized provincial screening program the Ontario Breast Cancer Program (OBSP) or through non-OBSP sites. OBSP offers important advantages for women and their primary care providers, including scheduling of all screening appointments, sending recall and result letters to women, and arranging follow-up services for women with results that show that they need more tests.
- Women who are screened for breast cancer within an organized screening program like the OBSP further benefit by participating in a program that undergoes ongoing quality assurance, program monitoring and evaluation to ensure that its clients receive high-quality screening. In addition, all OBSP sites are accredited with the Canadian Association of Radiologists Mammography Accreditation Program.
- For women aged 30-69 who have been confirmed to be at high risk for breast cancer, breast MRI in addition to mammography has been shown to be the most effective screening approach. The OBSP High Risk Screening Centres facilitate referrals for genetic assessment for women who may be at high risk for breast cancer (if appropriate). For women who have been confirmed to be at high risk for breast cancer, these centres offer annual screening mammography and breast MRI, and facilitate follow-up breast assessment services for women who require extra tests.
- An organized screening program can result in earlier detection of cancer and, as a result, better health outcomes. Cancer Care Ontario aims to increase the proportion of women who undergo breast cancer screening in the province, with a goal to reach more vulnerable populations, through supporting local and regional innovative approaches to screening.
- The Ontario Association of Radiologist supports breast cancer screening for women in their 40s
- The OAR endorses the Canadian Association of Radiologists’ (CAR); the American College of Radiology (ACR) and Respected International Radiologists’ position on breast screening for women in their 40s.
- Do not schedule your mammogram for the week before your period if your breasts are usually tender during this time. The best time to schedule is one week after your period.
- Always inform your doctor or x-ray technologist if there is any possibility that you are pregnant.
The ACS also recommends you:
- Do not wear deodorant, talcum powder, or lotion under your arms or on your breasts on the day of the exam. These can appear on the x-ray film as calcium spots.
- Describe any breast symptoms or problems to the technologist performing the exam.
- If possible, obtain prior mammograms and make them available to the radiologist at the time of the current exam.
- Ask when your results will be available; do not assume the results are normal if you do not hear from your doctor or the mammography facility.
- Before the examination, you will be asked to remove all jewelry and clothing above the waist and you will be given a gown or loose-fitting material that opens in the front
- You will be asked to change into a gown and remove your clothing from the waist up.
- The technologist performing your examination will review your mammography history form.
- A mammography procedure is relatively simple to perform, and technologists are specially trained to position you and the machine for the highest quality images possible. The mammography equipment may be tilted to improve the maximum exposure of your breast during image acquisition.
- The actual time required to obtain the necessary pictures of your breast is about ten minutes.
- The breast is first placed on a special cassette and compressed with a paddle. The technologist will take two images of each of your breasts, which will require the breast to be compressed for a few seconds during the actual x-ray portion of the exam.
- Although uncomfortable, the compression will not harm your breast in any way, and is necessary for optimal image acquisition. Be sure to inform the technologist if you experience pain during compression.
- After your examination is done, the technologist will have you wait in the gowned waiting room. It is necessary that you remain in the waiting room until the technologist reviews your films to ensure that additional images of your breast are not needed. After this review, the technologist will let you know when you can change and leave.
Benefits
- Imaging of the breast improves a physician’s ability to detect small tumours. When cancers are small, the woman has more treatment options, and a cure is more likely.
- The use of screening mammography increases the detection of small abnormal tissue growths confined to the milk ducts in the breast, called ductal carcinoma in situ (DCIS).
- These early tumours cannot harm patients if they are removed at this stage and mammography is the only proven method to reliably detect these tumours.
Risks
- The effective radiation dose from a mammogram is about 0.7 mSv, which is about the same as the average person receives from background radiation in three months.
- The Federal mammography guidelines require that each unit be checked by a medical physicist each year to insure that the unit operates correctly.
- Women should always inform their doctor or x-ray technologist if there is any possibility that they are pregnant.
- Five to 10 percent of screening mammogram results are abnormal and require more testing (more mammograms, fine needle aspiration, ultrasound or biopsy), and most of the follow-up tests confirm that no cancer was present.
- It is estimated that a woman who has yearly mammograms between ages 40 and 49 would have about a 30 percent chance of having a false-positive mammogram at some point in that decade, and about a 7 to 8 percent chance of having a breast biopsy within the 10-year period.
- The estimate for false-positive mammograms is about 25 percent for women ages 50 or older.
- Interpretations of mammograms can be difficult because a normal breast can appear differently for each woman.
- Also, the appearance of an image may be compromised if there is powder or salve on the breasts or if you have undergone breast surgery.
- Some breast cancers are hard to visualize, a radiologist may want to compare the image to views from previous examinations.
- Not all cancers of the breast can be seen on mammography.
- Breast implants can also impede accurate mammogram readings because both silicone and saline implants are not transparent on x-rays and can block a clear view of the tissues behind them, especially if the implant has been placed in front of, rather than beneath, the chest muscles.
- The NCI says that experienced technologists and radiologists know how to carefully compress the breasts to improve the view without rupturing the implant. When making an appointment for a mammogram, women with implants should ask if the facility uses special techniques designed to accommodate them.
- Before the mammogram is taken, they should make sure the technologist is experienced in performing mammography on patients with breast implants.
- Mammograms are the best way to find breast cancer early. However, they are not perfect. They may miss some cancers. Also, some cancers develop in the interval between screens. However, many studies have shown that regular mammograms reduce the risk of dying from breast cancer.
- Some cancers that appear on a mammogram may never progress to the point where a woman has symptoms during her lifetime. Therefore, some women may have surgery or treatment for a breast cancer that would never have been life threatening.
- Not all cancers found a screening can be cured. However, most women (88 percent) are alive and well five years after early detection and treatment of breast cancer.
- Mammograms are safe. Mammograms use a low does of radiation.
- The benefits of screening and finding cancer early are more important than any potential harm from the X-ray.
- A diagnostic mammogram is usually for a patient who finds a lump, has a breast problem, breast cancer or mastectomy.
- A negative mammogram means that the radiologist did not see any abnormalities in the breast tissue on the films.
- In general you should continue with monthly self-examinations, regular examinations by your physician, and have a mammogram within a year or two, depending on the guidelines suggested by your age and your personal physician.
- Unfortunately, mammography is not a perfect test: it does not detect all breast cancers either palpable or nonpalpable. This is particularly true if your breast tissue is very dense.
- It is important not to ignore a new breast problem, such as a lump, even if you discover it after a negative mammogram.
- An abnormal mammogram means that the radiologist has identified a “finding” on your mammogram. This abnormality requires further evaluation.
- The vast majority of such findings are benign or non-cancerous.
- Additional tests to evaluate irregularities in breast tissue include special mammographic views, ultrasound and biopsy. In breast ultrasound, the radiologist uses sound waves to produce images of the breast.
- With these images, the radiologist can determine whether a lump seen on the mammogram is a non-worrisome fluid-filled cyst, or a solid mass or complex cyst, which may require additional attention.
- Lumps that are solid (noncystic) often require biopsy to determine their origin.
- In a biopsy, tissue is removed from the lump and the surrounding area of the breast and is tested for malignancy.
- Biopsy may be performed with a large-gauge needle or by surgical incision, depending on the indications and patient and physician preferences.
- Ontario lags behind the rest of Canada in its adoption of digital mammography services. Where virtually every other province has made the investment in digital mammography as the new standard of care Ontario has no plan or stated policy.
- Approximately 60% of Ontario’s mammography equipment is still using X-ray film. The slowness to adopt digital mammography means that Ontarians are not being given access to more state-of-the-art technology as their provincial neighbours.
- The OAR continues to be concerned with the lack of breast screening using Breast Tomosynthesis, which is a promising technique that can only be used in tandem with FFDM equipment.
- It acquires multiple projections of a compressed breast from different angles. Images are re-constructed and can be viewed individually or dynamically. The new and improved images address many of the problems associated with conventional mammography. Part of the problem with mammographic images is that the breast tissue can obscure malignancies.
- In some mammographic images, normal tissue can appear suspicious, setting off a chain of additional imaging and patient anxiety. False-positives cost money, impact workflow and frustrate patients and physicians.
ADD VIDEO – The Value of Digital Mammography
- A new technology pioneered at Massachusetts General Hospital, breast tomosynthesis, also called 3D mammography, is a new type of mammogram that produces a three dimensional image of the breast and improves cancer screening and detection.
- A New Dimension in Breast Cancer Detection Conventional 2D mammography produces a single, flattened image of the breast, making it difficult for doctors to detect small cancers.
- Breast tomosynthesis minimizes the impact of overlapping breast tissue during imaging because the camera moves over the breast taking images from multiple angles.
- These images are combined to create a three-dimensional rendering of the entire breast.
- At this time, breast tomosynthesis in the United States is performed along with a standard mammogram on the same scanner.
- Tomosynthesis eliminates problems caused by the superimposition of normal structures.
- Tissue isnʼt sandwiched; it can be viewed layer by layer, much like the slices of a multi-detector CT or MRI study.
- The ability to view tissue layer by layer translates into important benefits. Most importantly, the ability to view individual layers is expected to reduce the callback rate because the radiologistʼs view of any suspicious area is not obscured by breast tissue.
- Radiologists should be able to detect more cancers, specifically those obscured (and missed) by overlapping tissue.
- Earlier detection is another strong advantage. It is likely that radiologists will find smaller cancers than they would with conventional mammograms.
- With breast tomosynthesis, specialized breast radiologists can manipulate the images to see areas of concern from all angles.
- Earlier detection of small breast cancers that may be hidden during 2D mammography
- Greater accuracy in pinpointing size, shape and location of abnormalities
- Fewer unnecessary biopsies or additional tests
- Greater likelihood of detecting multiple breast tumors, which occur in 15% of breast cancer patients
- The key to reducing breast cancer is to find an increasing number of smaller cancers.
- This is why The OAR is continuing to advocate for patients and radiologists and is committed to working with the Provincial Government to find solutions.
- Currently, no fee code exists for this new, life-saving technology in Ontario. There are only a small handful of hospitals that offer tomography breast screening including North York General and Princess Margaret Hospital.
- A breast ultrasound is another imaging technique to look at the breast.
- A gel is put on the breast to make it slippery and a small transducer is slid along the skin sending waves through it.
- A fine needle aspiration biopsy is a removal of a cell sample from a lump or area of concern using image guidance.
- These cell samples are reviewed by a pathologist and the patient is given a preliminary diagnosis after their exam.

- A core biopsy is a removal of a tissue sample from a lump or area of concern using image guidance.
- This tissue sample is sent to the pathologist for analysis.
- A cyst aspiration is the removal of fluid from a sac that grows in the midst of the breast tissue by attaching a needle to a syringe that is inserted through the breast.
- A galactogram is a procedure where a catheter is used to cannulate the milk duct. The radiologist injects a radio opaque dye into the duct to highlight any abnormalities.
- A needle localization is a procedure used to guide a surgical breast biopsy. A thin wire is used to show the lesion to the surgeon.
- It is placed in the breast under x-ray or ultrasound guidance. The wire is left in the breast when the patient goes to the O.R.
- Breast cancer is the most common type of cancer for women in Ontario
- In 2012, an estimated 9,100 Ontario women developed breast cancer and approximately 2,000 died from the disease
- Older women are at greater risk of getting breast cancer
- 80% of breast cancers are found in women aged 50 and older
- Most women diagnosed with breast cancer have no family history of the disease
- Less than 1% of women in the general population are estimated to be at high risk for breast cancer